Diabetes is on the rise globally. Since the 1980s the number of people living with the disease has quadrupled from 108 million to 537 million.
This dramatic increase is largely due to the rise in type 2 diabetes and its associated risk factors such as being overweight or obese.
For many years, diabetes was considered a disease of affluence and thought to be rare in sub-Saharan Africa. This is no longer the case. Today 24 million people – one in 22 adults in the region – have diabetes and rates are rapidly increasing.
In Liberia, one of the poorest nations in sub-Saharan Africa, it is reported that an estimated 2.1% of its population of 5.2 million are living with diabetes. More than half of them are undiagnosed, underscoring the grave burden of diabetes in the country.
Available research on diabetes in Liberia excludes people’s voices and stories. It is not rooted in people’s lived experiences. As a result, the research findings seldom lead to change.
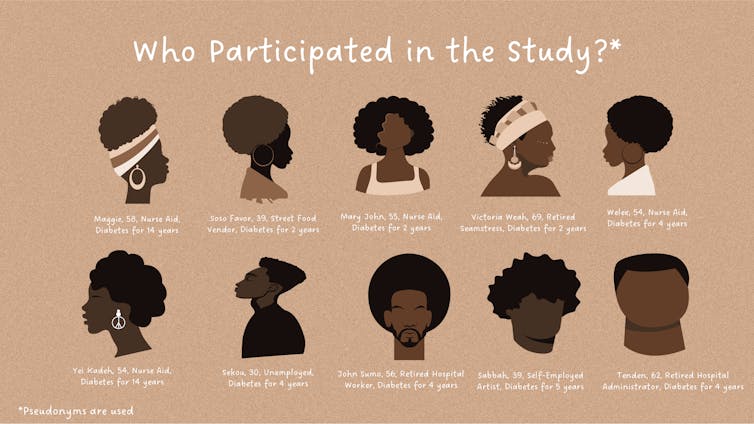
The goal of our study was to understand people’s lived experiences with diabetes in Liberia. We used a photovoice method, providing 10 Liberian adults with cameras to take photographs representing their lives. Through discussing the meaning of their photographs, we gained insights into local assets and needs.
Participants were recruited from Redemption Hospital in Monrovia. Due to COVID-19 restrictions, we partnered with Adventist University of West Africa to help facilitate interviews.
Our study identified two major challenges: food insecurity and healthcare neglect.
Worrying about the next meal
Participants shared stories about worrying about obtaining food, compromising the quality of food they ate, skipping meals and experiencing hunger. They were often forced to choose between food and medication.
Not taking medication regularly for diabetes can lead to dangerous consequences like severe hypoglycemia or hyperglycemia, coma and sometimes death.
One of the participants who was diagnosed with diabetes four years ago had diabetic retinopathy, a common complication of diabetes that leads to vision loss.
He had been unable to work since his diagnosis and relied entirely on his sisters for financial help and the kindness of friends in his community.
During periods of extreme financial hardship, the 30-year-old experienced hunger.
When I don’t have money, I don’t eat.
If people like him survive the short-term consequences of hunger, repeated experiences of hunger can also place people living with diabetes at risk for long-term consequences such as cognitive impairment.
Participants also reported concerns about the limited food options that healthcare providers recommended for their diet. They were generally advised to avoid staple foods with high glycemic indexes such as white rice and cassava dumboy that raise the blood sugar quickly and to replace them with foods like bulgur wheat and green plantain, as they provided better blood glucose control.
It was not always possible to adhere to these recommendations as foods like bulgur wheat and green plantain were far more expensive.
Back of the queue
Liberia’s 14-year civil war coupled with the Ebola outbreak left a devastating impact on the country’s healthcare system.
As a result the country faces unique challenges in combating diabetes because of the country’s limited health infrastructure, which neglects people living with chronic illnesses.
In 2018, only about 22% of publicly funded healthcare facilities could provide diagnosis and management of diabetes. This makes it very difficult, for example, to get basic diabetes care such as testing, medication and diabetes education.
Participants on the research attested to this. One voiced his frustration with the local hospital and the lack of supplies and resources allocated to people living with diabetes. He was particularly disappointed that his local hospital was routinely out of medications:
Sometimes at the hospital, they don’t have all the medicine. Yeah, so the whole frustrating part is when you get there, and the medicine not there, you have to pay for your prescription. With the prescription, he can just write it for me, and I will try to get it, because I want to be treated. They give you prescription, then you go to the drug store.
Participants also shared how their religious faith helped them cope and sustain hope of living with diabetes. Their transcendent hope persisted despite hardship.
The way forward
Our findings demonstrate the need to improve the health and quality of life of people living with diabetes in Liberia.
Based on our findings, we recommended the following:
-
Increased prioritisation and resourcing of diabetes management. This would involve allocation of adequate resources for screening, diagnostic testing, medications, diabetes supplies and diabetes education.
-
Integrated diabetes centres to facilitate ongoing care. To the best of our knowledge, there is currently no public or private diabetes centre in Liberia.
-
Community food programmes with healthy options. These should include community gardens and food banks.
Denial of responsibility! My Droll is an automatic aggregator of Global media. In each content, the hyperlink to the primary source is specified. All trademarks belong to their rightful owners, and all materials to their authors. For any complaint, please reach us at – [email protected]. We will take necessary action within 24 hours.